Hope for diabetics
Diabetes is still incurable. But with the help of data science, this could soon change. At MUDS, Karin Hrovatin is researching the cells involved in insulin production. The goal is to stimulate hormone production again in the future.
Even as a child in Slovenia, Karin Hrovatin liked to draw and do math. Her favorite exercise book in elementary school was called "Math is a Game"; it contained math problems to be solved by coloring pictures - she liked it so much that as soon as she finished her book, she started all over again in her classmate's book.
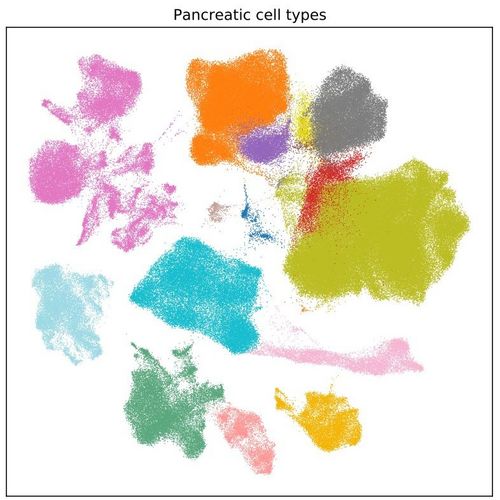
Today, Hrovatin is a doctoral student at the Munich School for Data Science (MUDS). But she still solves big problems with colors, drawings and visualization. "Most people think of Data Science in terms of programming, statistics and mathematics," Hrovatin says. "Yet visualizing through drawings or graphical representations is actually one of its most important aspects."
Using scatter plots that look like rainbow-colored clouds or abstract art, Hrovatin is addressing a problem that affects nearly one in 10 adults worldwide: diabetes, a chronic disease whose consequences can extend to amputations, blindness, heart attacks and strokes. "Diabetes is a highly problematic disease," says Hrovatin, "and very widespread, so finding a solution is a really important research topic."
Better understanding the body's insulin factory
Hrovatin first studied biotechnology at the University of Ljubljana and then bioinformatics and diabetology at the University of Edinburgh. In the process, she found that she was more interested in numbers than practical lab work. Nevertheless, the Slovenian data scientist wanted to continue researching diabetes, one of the most pressing public health problems today.
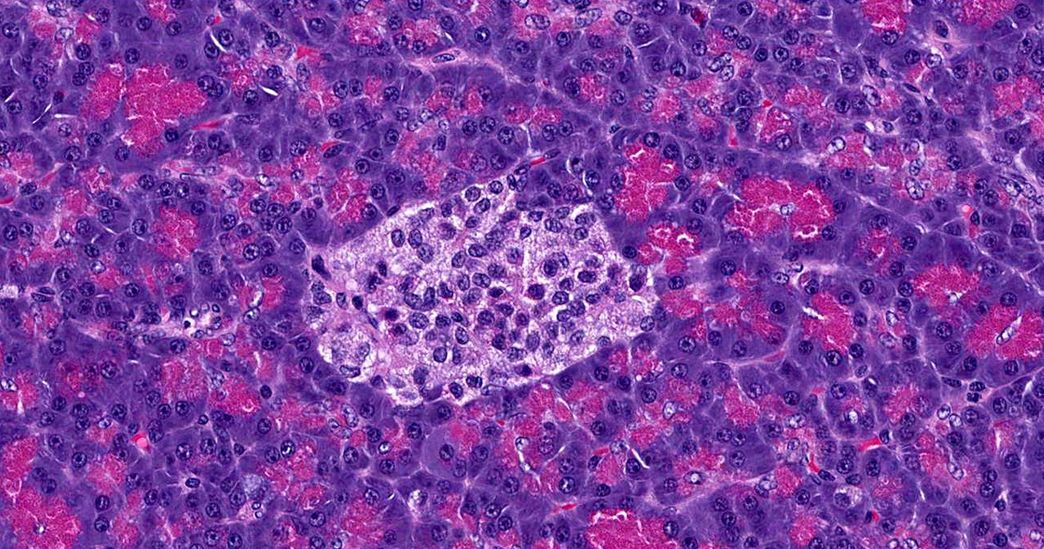
Thanks to a unique interdisciplinary data science program of the Helmholtz Association, she can combine the two and use cutting-edge data science methods to better understand the progression of diabetes at the cellular level. As a PhD student at the Helmholtz Information and Data Science Academy's Munich School for Data Science, Hrovatin is working to better understand beta cells, the body's insulin factories. Beta cells are located in the pancreas and respond to rising glucose levels in the bloodstream, the blood sugar level, by producing the hormone insulin. This, in turn, signals muscle cells to absorb blood glucose and store it for later use.
However, if the beta cells are defective, they no longer produce enough insulin - and the body no longer absorbs blood sugar. This results in type 2 diabetes, one of the most common and fastest spreading non-communicable diseases in the world today.
Why do beta cells stop functioning?
In order to one day be able to cure diabetes, researchers are trying to better understand why beta cells stop functioning. Until now, it was assumed that they have to work too hard on a diet too rich in sugar and at some point simply become exhausted.
However, it is now known that not all beta cells are the same. They differ from person to person and even between neighboring cells. Understanding how beta cells tick - and sometimes stop ticking - is the focus of Hrovatin's work.
While scientists previously assumed that retired beta cells were beyond repair, recent discoveries show that some of them can indeed be revived. However, it's not yet clear which ones will respond to treatment. "Beta cells change during the aging process or due to stress. We are looking for differences between healthy and diseased beta cells to figure out how to regenerate them or make them work again," Hrovatin explains. "If it were possible to restore beta cells to their healthy state, this could restore their function in the pancreas."
An "atlas" of insulin-producing beta cells
The lab at Helmholtz Zentrum München's Institute for Computational Biology, where she works, focuses mainly on single-cell sequencing, a data analysis technique that allows biologists to directly study cell properties in mice with diabetes. Despite its huge potential, the research takes place at the microscopic level: Hrovatin's colleagues take cells from the pancreas of rodents and isolate individual cells from the organ tissue, whose properties and response to treatments and stress they then study.
The beta cells are lined up in a tiny tube, individually enclosed in oil droplets and each marked with a unique identifier. A data set can be based on as few as 10,000 cells, a quantity that is barely visible to the naked eye.
Hrovatin's ultimate goal is to combine data from many different cell types and experiments to create a kind of "atlas" of beta cells to understand which cells share common characteristics and how their metabolic function differs. On this basis, scientists may be able to develop better, more individualized treatments for type 2 diabetes in the future. The Helmholtz Diabetes Center is a leader in this area of research. "There is already a lot of data available, so diabetes is well suited for data analysis," Hrovatin explains.
Using machine learning and data science, Hrovatin wants to analyze which cell properties different disease types and treatments have in common - creating a kind of atlas of cell subtypes. "I could use this information to predict how cells in a living organism are likely to respond to a treatment," she says, "based on how they respond in cell culture." That, she hopes, will be an important first step toward developing therapies for diabetes patients.
Making data sets comparable
Before it can make meaningful comparisons of cell types and functions, however, it has to make sure that the data sets match up at all. In an ideal world, all researchers would base their experiments on the same methods, so it would be easy to compare results and see how cells respond to different types of stress and treatments.
But we don't live in an ideal world. When Hrovatin arrived in Munich this summer, she realized the extent of the problem: "There are different mouse models, different types of disease, different lab protocols," she explains. "There are lots of differences, and that's a big challenge."
That's why she devoted the first four months of her doctoral research to figuring out how to match data sets so that cells can be compared in a meaningful way. "It's important to match datasets, but first you have to make sure you're actually analyzing biological effects and not technical ones," Hrovatin says. "I hope to verify the results in collaboration with biologists." So far, she has already been able to draw on the expertise of diabetologists and bioinformaticians at Helmholtz Zentrum München.
Interdisciplinary inspiration from the MUDS
The Alpine backdrop of Munich reminds the Slovenian scientist of her hometown of Ljubljana, the capital of Slovenia. She enjoys exploring the city by bike - and riding to her lab, despite the unusual conditions and limited contact during the Corona pandemic. Meanwhile, at MUDS, there is a growing network of graduate students with similar research interests.
As part of the Helmholtz Information and Data Science Academy, MUDS is a link between Helmholtz Zentrum München, the Max Planck Institute for Plasma Physics and the German Aerospace Center. Among Hrovatin's colleagues are experts from the fields of robotics, plasma physics and biomedicine - they all share a focus on new applications for Data Science. While the doctoral students can't meet in person, they regularly come together online in seminars. "It's great," Hrovatin finds, "I can learn from people in other fields and get ideas that I can apply to biology."
Hrovatin still finds time for her childhood passion of drawing. In her spare time, for example, she designs imaginative fashion and haute couture. But her energy now goes into another form of art: colorful visualizations of data points and cell types that she hopes will one day cure diabetes patients.
Author: Andrew Curry